
2020. Proof that challenge makes us stronger.




“No matter what, we are resilient and ready to take on any challenges we may face as educators and care providers.”


In the face of pandemic, civil unrest and economic crisis, we brought our communities science, invention and compassion. This past year has made us stronger than ever, and has proven the power of resilience. From here, we can take on anything.
 I am proud of the VCU Health community’s unwavering resilience and dedication to education, treatment and care for all who come to our health system. They are what the world needs now, and I am grateful for their resilience and compassion.
I am proud of the VCU Health community’s unwavering resilience and dedication to education, treatment and care for all who come to our health system. They are what the world needs now, and I am grateful for their resilience and compassion.
This annual report comes to you during a challenging time to our communities and our nation. No matter what, we are resilient and ready to take on any challenges we may face as educators and care providers. The stories in the report offer a brief glimpse into some of these challenges and our work to examine, educate and treat those we serve.
I am grateful for the leadership of now-retired VCU Health System CEO and Senior Vice President Marsha Rappley. Because of Dr. Rappley’s dedication to serving the community, we are able to provide individualized care space to our youngest community members and are even closer to reaching our goal of state-of-the-art facilities for adult patients.
School of Medicine Dean Peter Buckley led with great care as interim senior vice president and CEO. His unwavering focus on patient safety, quality care, service and accessibility during a year of change was exemplary.
Building on the great work of Drs. Rappley and Buckley, Dr. Art Kellermann assumed the role of senior vice president for health sciences and CEO of VCU Health System in October. I am pleased that he will continue to foster work across disciplines in our effort to provide world-class care to all who come to us for service and treatment.
Thank you for your continued support of VCU.

Michael Rao, Ph.D.
President, VCU and VCU Health System
The world paused, but our research never stood still.
VCU posted an institutional record of $335 million in sponsored funding in fiscal year 2020, an 8 percent increase over the previous year. More funding means more medical breakthroughs.

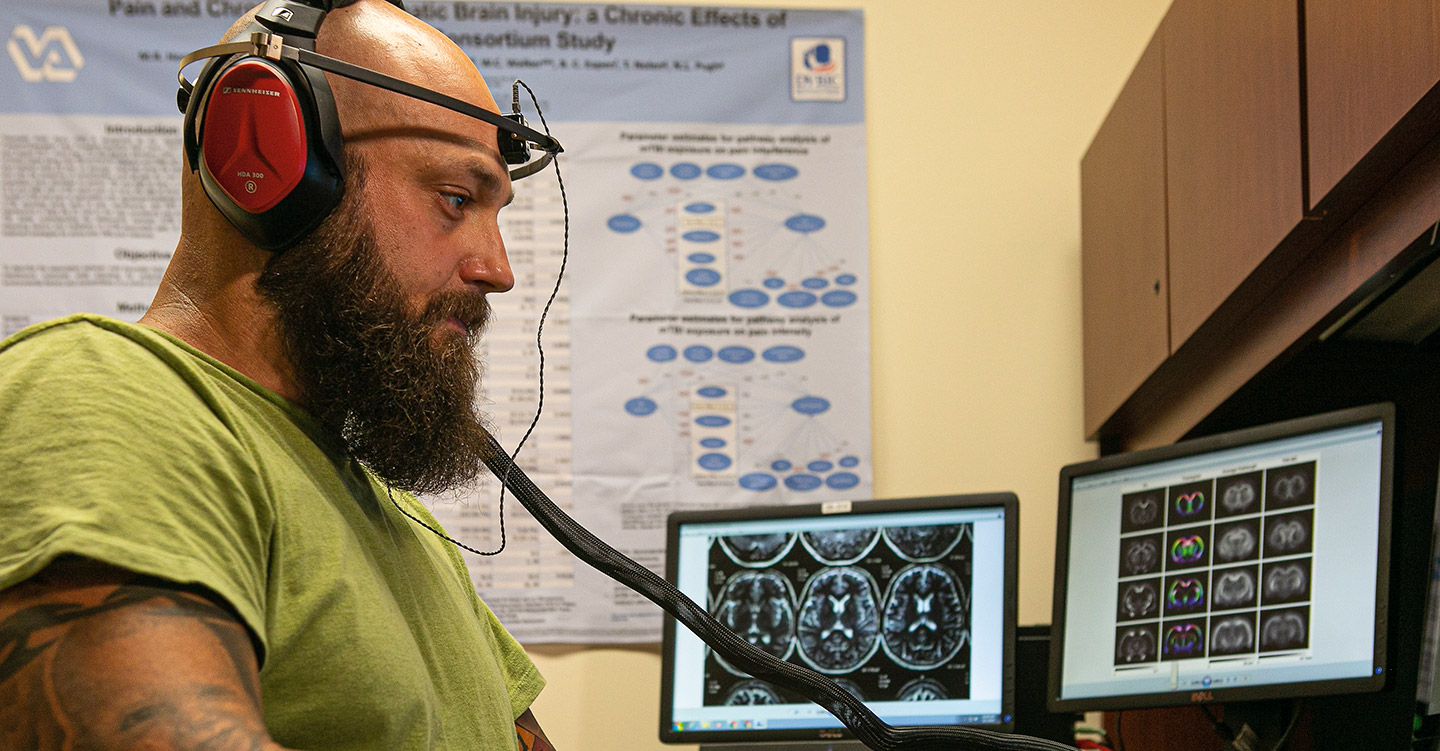
Virginia Commonwealth University has been awarded a $50 million federal grant to oversee a national research consortium of universities, hospitals and clinics studying the long-term impacts of mild traumatic brain injuries or concussions on service members and veterans.
The Long-term Impact of Military-Relevant Brain Injury Consortium (LIMBIC) focuses on the ongoing health impacts of combat concussions, such as those from blasts, bullets and hand-to-hand fighting as well as vehicle accidents, sports injuries and falls. Researchers from the LIMBIC team have already discovered links between combat concussions and dementia, Parkinson’s disease, chronic pain, opioid usage and suicide risk.
The principal investigator on the grant is David X. Cifu, M.D., professor and chair of the VCU School of Medicine’s Department of Physical Medicine and Rehabilitation and senior traumatic brain injury specialist for the U.S. Department of Veterans Affairs.
“We are getting a 360-degree overview of all aspects of these veterans and service members, from their brains and nervous systems to their emotional well-being to their day-to-day functioning,” Cifu said. “This is the largest study of its kind that is entailing a deeper dive and more thorough investigation than any person, patient or even research participant could get.”
The Departments of Defense and Veterans Affairs are funding the grant, which will bring together universities, Veterans Health Administration hospitals — including Richmond's Hunter Holmes McGuire VA Medical Center — and the military to study the impact of combat concussions. This new LIMBIC research, which launched Oct. 1, 2019, will continue for five years.
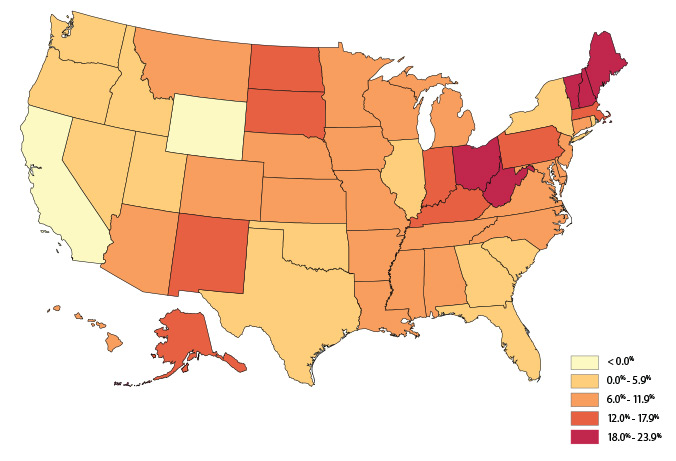
Even before the pandemic, mortality rates among working-age Americans continued to climb, causing a decrease in U.S. life expectancy that is severely impacting certain regions of the United States, according to a 2019 Virginia Commonwealth University study. The report, “Life Expectancy and Mortality Rates in the United States, 1959-2017,” is one of the most comprehensive 50-state analyses of U.S. mortality.
Published in JAMA in November of 2019, the study found that deaths among Americans ages 25 to 64 are increasing, particularly in Rust Belt states and Appalachia. This “distinctly American phenomenon” has fueled a decline in U.S. life expectancy since 2014, and is linked to several major causes of death outside of COVID. Compared to the 1990s, working-age adults are now more likely to die before age 65 from drug overdoses, alcohol abuse and suicides — sometimes referred to as “deaths of despair”— but also from an array of organ system diseases. Mortality rates have increased for 35 causes of death, said lead author Steven Woolf, M.D., director emeritus of the VCU Center on Society and Health.
Some of the largest increases in working-age mortality since 2010 occurred among women and adults without a high school diploma. The industrial Midwest and other regions that have been hard-hit by changes in the economy since the 1980s are experiencing the largest increases in mortality.

In early 2019, VCU launched a three-year, $7 million initiative to support the development of new innovations in health care. The Health Innovation Consortium will tap into the rich resources of VCU faculty research, talented students and VCU Health in partnership with Richmond’s entrepreneurial ecosystem to solve problems in health care through innovation.
“This consortium will allow students or faculty who have an idea to innovate health care to move seamlessly from concept to commercial viability to mature startup,” said VCU President Michael Rao.
In support of the initiative, VCU Health will invest $2.5 million per year over the next three years. That investment will fund operations, and support a pre-seed fund and seed fund to help bring the innovations to market and potentially launch startup companies.
The consortium has been an active part of COVID-19 response in the region, supporting the design and implementation of VCU Health’s N95 Decontamination facility; working with community innovators to prototype and deliver face shields to various VCU offices; and filling gaps in the community via mask manufacturing, ventilator prototyping, and a series of other innovative, impact-driven projects. The consortium was recently a recipient of Richmond’s 2020 Inno on Fire Blazer award.

During his childhood, Virginia Commonwealth University School of Dentistry student Chase Phillips recognized how welcoming and comforting his family dentist was. Today, he’s studying the comfort levels of fellow members of the LGBT community, in his research project, “Identifying Oral Health Priorities, Use of Services, and Inclusive Understanding of Oral Health Providers among the LGBT Community.”
Phillips chose to explore the topic after realizing that no previous research had detailed the viewpoints of LGBT patients about the dental care experience.
“As a member of the LGBT community myself, I know how important it is to feel safe in any kind of medical environment,” Phillips said. “Going in can be stressful for anyone, but then having to worry on top of that if there might be another issue that arises based on your sexuality can make it even more stressful.”
Research has long interested Phillips, who earned bachelor’s and master’s degrees in psychology at the College of William and Mary and Villanova University and who worked in special education before deciding to attend dental school. He chose the VCU School of Dentistry in part for its strong student research culture.
The project will combine individual interviews of stakeholders in the LGBT community with a broader survey of the community using themes developed from the interviews — a mixed-method approach that should yield qualitative and quantitative results from the community’s perspective. Phillips said initial interviews for the project have pointed to an array of possible challenges, ranging from cost to medical anxiety and fear of discrimination.
Philips was awarded a Student Research Fellowship from the American Association for Dental Research for the project.

Caring and compassion proved their power.
We faced a medical crisis of epic proportion. Still, we know that health care is all about individuals. The success of our patients and their families continues to drive us forward.

With eight children and 21 grandchildren, family is everything to Edward Foster. And when Foster needed his family the most, they were certainly there for him.
For decades, the 69 year-old had battled a chronic disease that was pushing his liver to failure. He suffered from primary sclerosing cholangitis, a condition in which the body attacks and inflames the bile ducts and causes liver failure. He was faced with possibly months, if not years, on the national transplant waitlist. But there was another option — a living-donor liver transplant.
The procedure is complex, and involves a multidisciplinary team of specialists. For the donor, the surgery entails removing part of the liver, which is then transplanted into the recipient. According to David Bruno, M.D., surgical director of adult and pediatric liver transplantation at the VCU Health Hume-Lee Transplant Center, “It’s nothing short of a heroic act.”
Members of Foster’s large family were more than willing to donate. After a number of tests, his youngest son, 40-year-old Edward “Rick” Foster Jr., was a match. VCU Health’s team went into action.
The transplant team included living-donor liver donation expert Vinay Kumaran, M.D., whose resume includes more than 700 living liver donor cases. Kumaran and the Hume-Lee team removed the right lobe of Rick Foster’s liver and transplanted it into his father. Both father and son spent time recovering in Hume-Lee’s dedicated transplant unit with family members by their sides.
The procedures marked the first living donor liver transplant at VCU in nearly five years — and they also marked another chapter in the Hume-Lee Transplant Center’s storied history of transplantation, which includes Virginia’s first liver transplant and the first-ever “reduced-size” orthotopic liver transplant using a liver from an unrelated living donor.
“I appreciate everything they did for me,” Edward Foster said of the VCU team. “They became part of [my] hospital family.”

A recent paper by VCU College of Health Professions expert Laura McClelland showed that leading and creating systems of compassion results in better care. McClelland, an associate professor, found that compassion’s many benefits include easing stress and fostering an atmosphere of caring and collaboration. Her paper, “Actions, Style and Practices: How Leaders Ensure Compassionate Care Delivery,” was recently published with Timothy Vogus, Ph.D., of Vanderbilt University.
According to McClelland, “Compassion functions like an antidote. It buffers employees from stress and strain on the job and also helps people recover when they aren’t at their best. Leaders can set the tone, and they can create the scaffolding that ensures that compassion happens.
“Every day we hear stories of how compassion heals, helps and uplifts us as individuals and as a society. These stories continue to show us that when we lead with compassion, when we look out for one another, we are all stronger and more resilient because of it.”
With efforts such as The Pause to honor a patient’s death and Schwartz Rounds to allow health care workers to process the emotional consequences, VCU Health puts these principles into practice, said Lisa Ellis, M.D., executive director of patient and provider experience at VCU Health. “VCU Health leadership teams are embracing this with a systems-wide approach to mitigating burnout. We are on the path to openly aligning value systems and enhancing purposeful psychological safety approaches.”

Children’s Hospital of Richmond at Virginia Commonwealth University has launched a partnership with McGuireWoods and Dominion Energy to make an additional 50 attorneys available to families with legal needs that impact the health of their children. This relationship significantly expands the existing Medical-Legal Partnership — Richmond program, which began in January 2018 and offers free legal advice and representation for eligible patients and families in Richmond and surrounding counties.
With the addition of these attorneys, MLP-Richmond has expanded to provide access to legal counsel at no cost to families of pediatric patients at CHoR’s Virginia Treatment Center for Children and Brook Road Campus, along with adult patients at VCU Health’s Complex Care Clinic.
For the mother of a one year old with cerebral palsy, this legal assistance has proven vital to her son’s health. When her apartment had an unpleasant smell and was overrun with rodents, her already-fragile son experienced recurrent illness. She tried many times to get the general manager to take action without success. Their pediatrician at CHoR referred them to MLP-Richmond.
“Within a month, the attorney got us out of the apartment and into a new one. She even got my rent reduced at the new apartment to match what I was paying before,” said the mother. Her child has not been sick in months and is no longer on supplemental oxygen.
For our students, 2020 was a lesson in resilience.
The pandemic came to the forefront this year, but our faculty and student body proved their tenacity, gaining knowledge in crisis mode and adjusting to new ways of learning.

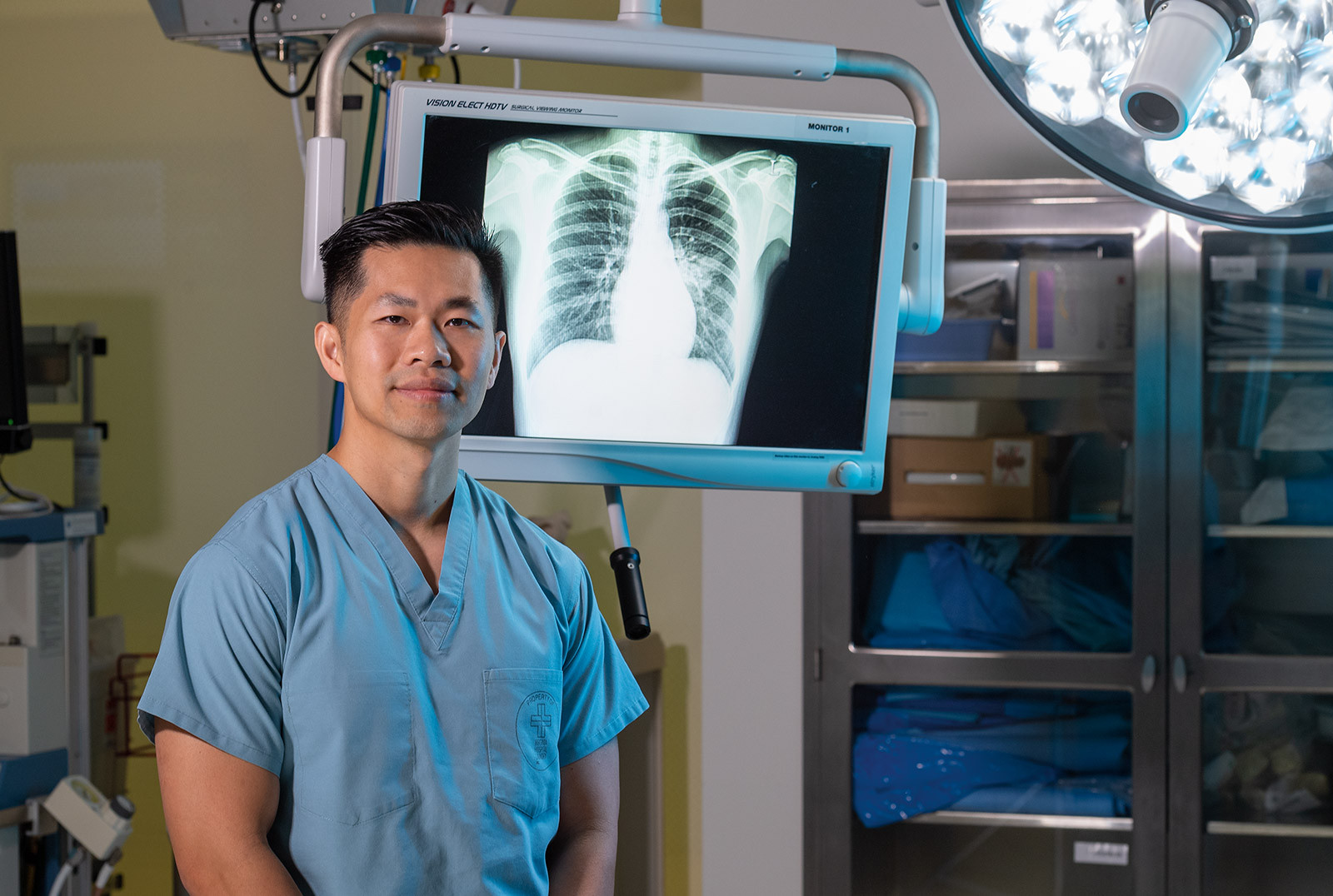
This is what determination looks like: When Jay Pham received his assignment on Match Day this year, it was the result of a lifetime of hard work. Pham, a fourth-year med student at VCU School of Medicine, was awarded his first choice: a residency at VCU Health in the Department of Radiology. The road to get there was a long one.
Pham’s story began in a small village in Vietnam. He recalls, as a child, traveling 4 hours with his father to Saigon, where his father’s doctor would get X-rays to track the progress of his tuberculosis. Jay, his parents and three siblings immigrated from that small village to the U.S. when he was 10 years old.
As a young man, he settled in Seattle, where he owned a number of nail salons. The recession of 2008 hit his businesses hard. In the face of that downturn, he told his wife, “I want to be a medical doctor.” He went on to earn a bachelor’s degree at the University of Washington in 2012, then applied at VCU School of Medicine in the radiology department. Says Pham, “My wife supported me, and we sold everything and came here.”
With five children, the Phams pushed forward, through financial challenge. To help with his finances, he received a scholarship made possible by the Dr. Arthur Kirschbaum Memorial Fund. As for time management, Pham credits his wife, Pa, for taking the lion’s share of the parenting responsibilities. “She makes sure I have time to study, and if I have to take extra time, she will take the kids. She also works full time at a nail salon and teaches at beauty school,” he said.
Along with his extensive studies and role as a father, Pham also finds time to give back. He serves as a tutor for the Premedical Graduate Sciences Certificate Program, and has volunteered at the CrossOver Healthcare Ministry since 2016. To Pham, “Volunteering at CrossOver allows me to stay true to my vow to help my community.” We are fortunate that Jay Pham has made our community his.

Growing up in the coal mining town of Lebanon, Virginia, Anesa Hughes would accompany her mother to community clinics, camping out in their car to get free health care offered to those without insurance. Her mother’s role evolved into full-time caregiving, as Anesa’s twin sister struggles with cerebral palsy and other health issues requiring 24-hour care. Anesa knew she would have to pursue an education, not only to help people medically, but also to contribute to her family’s finances, and support her sister later in life.
A neighboring pharmacist suggested she consider pharmacy school. After earning a B.S. in biology at King University in Bristol, Tennessee, she entered VCU School of Pharmacy. As a student, she was able to come back to Appalachia to provide care through the RAM/MOM program. She earned a doctorate in pharmacy in 2018, and completed her residency at the James H. Quillen Veterans Affairs Medical Center in Johnson City, Tennessee — not far from her family’s mountain home. Today, she works there full time as a clinical resident. “I feel that rural communities really lack health care,” said Anesa. “Just being able to provide health care to these people is part of my overall goal.”
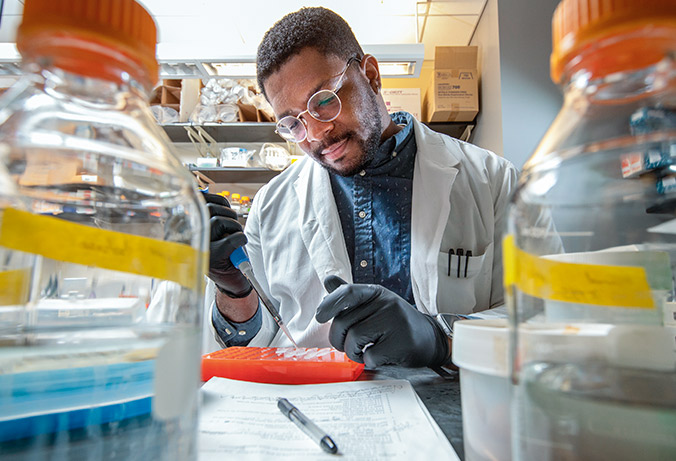
A new $2.5 million grant was awarded to VCU in 2019 by the NIH’s National Institute of General Medical Sciences, ensuring that the VCU Institutional Research and Academic Career Development Awards will continue supporting fellows through 2024. This three-year postdoctoral program is one of a number of efforts of the School of Medicine’s Center on Health Disparities, which was founded in 2005 to identify the causes of and develop interventions to eliminate inequality in health care.
The center works to tap into missing potential in underrepresented groups by training future biomedical researchers at the undergraduate, postbaccalaureate, graduate and postdoctoral levels. VCU is one of only two institutions in the U.S. to offer these programs at all levels.
Within the Center on Health Disparities’ program for undergraduates, 98 percent of participants in that program, who also are from underrepresented groups, have earned a bachelor’s degree. Twelve out of 14 postdoctoral trainees have entered tenure-eligible positions, 88 percent of participants in the undergraduate program are pursuing careers in the biomedical workforce, and 90 percent of postbaccalaureate students enrolled in Ph.D. programs since 2011 have earned their degree or are still actively pursuing it. Meanwhile, a national study conducted by the Council of Graduate Schools found that less than 60 percent of African American and Hispanic students enrolled in doctoral programs earned the credential within 10 years.

As an “activist researcher,” Dr. Kristal Brown examined, through her dissertation, the role of race-related discrimination in obesity and cardiovascular disease risk among young African American women. Brown, who completed her doctoral degree in social and behavioral sciences in the Department of Health Behavior and Policy at VCU School of Medicine, wanted to develop a community project that would highlight the lived experiences of young Black women. She worked with a local artist to take her conversations off the pages, transforming sentences and audio recordings into a mural that visually highlights the experiences of Black women.
“When you think about my dissertation, it is all numbers,” Brown said. “Whereas in my community project, not only does it parallel my dissertation, but it’s a narrative…it puts voices to the numbers that I am analyzing over here.”
With support from a grant last year from Initiatives of Change and the W.K. Kellogg Foundation, Brown developed the Brown Girl Narratives project under her Black Women Cache LLC, which focuses on highlighting the experiences of Black women. She led discussions with Richmonders about experiences of discrimination, which inspired the creation of the Brown Girl Narratives mural at 1125 Hull St. in Manchester. To create the mural, she worked with Austin Miles, a VCU School of the Arts graduate and artist.
“I was a part of one of those discussions,” Miles said. “I am a Black woman who has experienced racial trauma. And body image is a huge thing that I discuss in my work and being comfortable in your body. So it ties together.”
Today, the work of Brown and Miles stands tall, with images of seven diverse Black women staring out at the viewer. Their faces are framed by large sprays of dogwood flowers and the Richmond skyline appears behind them. The mural includes words and phrases from the conversations Brown led: “Superwoman,” “We are shaping our narratives,” “I am living the legacy of my ancestors,” “The audacity to be great,” “Courage,” “Overcoming anything,” “All shapes and sizes,” “Trendsetters,” “Strength,” “We have to work hard for everything,” “I wouldn’t want to be anything other than Black,” and “Beauty that can’t be defined.”
The virus struck.
We struck back.
The COVID-19 pandemic sparked invention, research, support and compassion throughout VCU Health. Our teams led the way, with clinical trials, testing and breakthroughs in patient care.
This April, Virginia Commonwealth University Health System launched a pilot program to safely decontaminate N95 masks using equipment and a method developed by VCU Health and VCU Ventures. The process can effectively decontaminate approximately 12 times the number of masks VCU Health currently uses daily.
As the COVID-19 pandemic has caused increased demand for N95 masks, this independently developed method of decontaminating and reusing masks allows VCU Health to replenish its own supply, providing the equipment necessary to keep its employees safe.
VCU’s decontamination process uses high-intensity ultraviolet light, an effective means of sterilizing hospital environments such as patient rooms and operating rooms. Before the masks are returned to the original user, they undergo a strict series of quality checks, including testing for moisture, penetration, fit and breathability.
While other approved methods of decontamination for the masks — such as using alcohol or steam — can work, they can also compromise the integrity of the masks after one or two uses. VCU’s process makes the masks reusable multiple times.
The decontamination method can be adapted by health systems across the country.
Project collaborators comprise researchers and staff from the VCU Health orthopaedic surgery, infectious diseases, supply chain, high-level disinfection and plant operations departments; VCU Ventures and the VCU da Vinci Center for Innovation.

When VCU School of the Arts alum Keith Ramsey was asked to use his welding expertise to help fight COVID, his immediate answer was “yes.” Ramsey was called on to build frames that would be used in VCU’s pilot program to decontaminate N95 masks, which are essential to health care workers.
The process uses equipment and a decontamination method designed by a team of VCU Health staff and researchers. This method allows VCU Health to replenish its own supply, by decontaminating more than 12,000 N95 masks a day. “That almost brought me to tears,” Ramsey said of hearing how the decontamination process will help prolong use of the masks. “It was amazing to me.”
Ramsey, who graduated from the VCU School of the Arts in 1998 with a bachelor’s degree in painting and printmaking, quickly jumped into action when he was delivered the metal for the project in March. “I had to build out the frames and then weld them together and also weld seven bars in the middle,” Ramsey said. “Then I put the casters on. It was like making a machine shop out of my workshop.”
He had to build a jig — a device that helps hold and guide the tools he was using — for the casters so he could drop them in before welding, and he also built a jig for the frame and one for the drill presses. Ramsey worked nine-plus hours a day to complete the project, and had the frames delivered to VCU on April 3.
“It was definitely the most meaningful project, because it has a direct outcome on society. It has a real purpose,” he said.
After finishing the project, Ramsey said he was “over the moon.”
“It was very rewarding,” he said. “If they ask me to do something again, there is no question that I’m going to do it.”
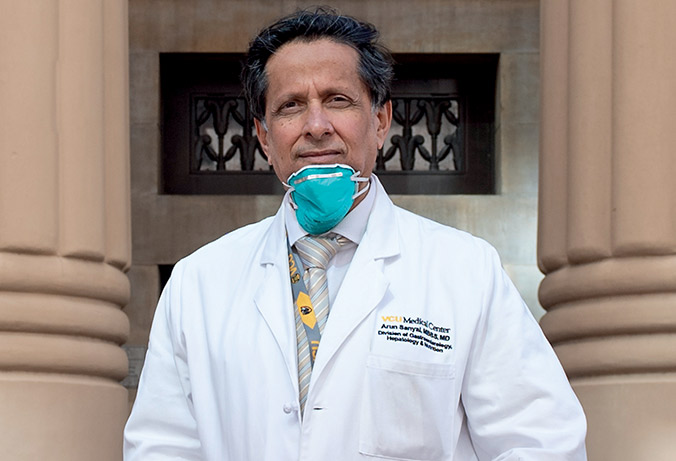
Virginia Commonwealth University researchers were fully engaged in the fight against COVID-19 this year, participating in clinical trials and statewide testing.
Led by principal investigator Arun Sanyal, M.D., VCU Health took part in two clinical trials for remdesivir, an experimental treatment for COVID-19. VCU was one of the handful of institutions in the United States to make these clinical trials available to patients who met the criteria for this investigational drug. The trials were a chance not only to provide access to remdesivir, Sanyal said, but also to generate data on the investigational drug’s safety and effectiveness. Two levels of acuteness were tested: moderate and severe, the latter defined as “someone whose symptoms require them to be on supplemental oxygen,” Sanyal said.
In May, the U.S. Food and Drug Administration issued an emergency use authorization for remdesivir for the treatment of suspected or confirmed COVID-19, one of just six emergency use authorizations granted and active as of September 2020.
VCU Health was also one of five sites across Virginia that collected antibody testing results as part of a statewide initiative to estimate how many people have been infected with COVID-19. VCU Health coordinated antibody testing, also called serology testing, for the state’s central region of the Virginia Department of Health (VDH) through the Virginia Coronavirus Serology Project. A COVID-19 antibody test checks to see if you’ve developed an immune response to COVID-19.
The study was conducted from June to August 2020. Results showed that an estimated 2.4% of adult Virginians have antibody test evidence of a prior COVID-19 infection. The presence of COVID-19 antibodies was highest in Hispanic individuals (10.2%), residents of the Northern region (4.4%), and among those uninsured or insured through Medicaid (3.8%). People who test positive for COVID-19 antibodies may be able to donate antibody-rich plasma, which could possibly save someone’s life.

For Kathy White, it all started with a rash. It was March 2020, the early days of the COVID-19 outbreak in the U.S. Her symptoms quickly worsened. Suddenly, her body temperature wouldn’t regulate, and as she says, “I just kept coughing.”
One night she woke up to a sensation she said she’d never forget. “I got up, and it was like the change in altitude on a plane. The weight of the air was on my chest, and I couldn’t breathe,” she said. She fell and injured her ankle. She tried calling out to her husband, but she couldn’t scream. That’s when she dialed 9-1-1.
At VCU Health, White was diagnosed with COVID-19. The damage to her lungs made talking exhausting. Trying to maintain a positive outlook added to her fatigue. She credits VCU Health nurses for getting her through the lonely, isolating experience of hospital quarantine. “I had four nurses,” White said. “I don't think I would have pulled through if it weren't for them.”
During her hospitalization, she enrolled in the sarilumab trial at VCU, one of several active clinical trials for COVID-19 patients. Sarilumab is approved to treat rheumatoid arthritis, a disease that causes inflammation. Researchers hope it can reduce the dangerous inflammatory effects of COVID-19 on the lungs and keep patients off a ventilator.
“We’re so grateful to patients like Kathy for joining in these trials,” said Antonio Abbate, M.D., Ph.D., a co-investigator on the sarilumab trial and an associate director at the C. Kenneth and Dianne Wright Center for Clinical and Translational Research. “The data we can contribute with the help of volunteers like Kathy are invaluable.”
From the start of the global pandemic, VCU Health clinicians, with the help of the Wright Center, have moved quickly to bring experimental drugs like sarilumab to the hospital for clinical trials. Nearly all VCU Health patients with COVID-19 have volunteered for a trial. For Kathy White, within a week, her lung function started to improve.

A VCU School of Medicine student is one of three experts providing information to the World Health Organization on the United States’ health policy response to COVID-19. Second-year medical student Mathew Alexander has joined two professors from the University of Central Florida as “country experts” on the U.S. for a WHO initiative called the Health System Response Monitor, which collects data on how countries around the world are responding to COVID-19.
“This is meant to be a tool for policymakers and health systems leadership to not only inform their decisions in the [present] but also to look back in the future and understand ‘What were some of the best strategies for containing, for testing or for mitigating the spread?’” Alexander said. “As we’re reopening economies and reopening businesses, schools and other public places, what are some of those capabilities that countries will need to respond to pandemics in the future as well to respond to COVID-19?”
The Health System Response Monitor reports give context to the story behind the numbers, Alexander said. “A lot of the talk right now has been about case counts and death counts and comparing those [between] countries,” Alexander said. “But one of the reasons why this work is really important is because it gives you a better understanding of why countries may have acted the way that they did and different factors that influenced their decisions.”
Alexander has been working on health policy research since his undergraduate days at VCU. Combining his interests in medicine, business and policy, he also worked as a research assistant studying Medicaid expansion and its impact on substance use disorder treatment in Virginia.
To VCU Massey Cancer Center Director Robert Winn, M.D., information is a powerful tool in the fight against COVID. But as the impact of the disease progressed, he realized that timely and accurate facts about COVID-19 were not getting out to area churches. He stepped in and formed a partnership with Black clergy, and started a series of conference calls named Facts and Faith.
During the weekly calls, Winn provides the latest numbers and facts on the virus along with ways churches can keep their congregations safe. “It wasn’t evident what our African American communities were supposed to do. People were frightened and confused,” Winn said. “There was a myth that African Americans couldn’t get COVID-19. We at Massey Cancer Center and VCU Health wanted to bust the myths.”
One question that Winn hopes can be addressed is why African American communities seem to be hit harder with the virus. “Quite honestly, it’s more about the ZIP code,” he said. “That’s more important than the DNA.”
According to Winn, there have been disparities in some communities for decades. “You have social deterrents such as health, housing and education, as well as the socioeconomics of neighborhoods,” he said. “As a result, you have poor and underserved communities.” In principle, social distancing helps slow the spread of COVID-19, but only if you have space to create distance, Winn said. “When you have a large number of people living in a house, or people living on top of one another, social distancing isn’t possible.”
The weekly conversations Winn has with the clergy have covered everything from proper personal protective equipment and social distancing to how churches can open their doors safely. The number of participants on the Facts and Faith calls has grown from about 30 to hundreds, Winn said. “This is a great example of being community activated.”

Of the many individuals of Latinx origin in our region, about 36 percent speak predominantly Spanish. So when COVID-19 came to the forefront, VCU Health’s communications team knew it had to take action to ensure that care and resources were available to this important part of our community.
From April through July 2020, the team published more than a dozen articles in Spanish on the VCU Health News Center, produced five Spanish-language videos, distributed two waves of resources in Spanish to media outlets, held a live event and offered PDF resources on forwardrva.com.
A COVID-19 resource center on VCUHealth.org now provides updates and COVID-19 educational resources in Spanish, and COVID-19 resources are also shared in Spanish on VCU Health’s social media channels. Videos have been created to debunk COVID-19 myths, show people how to safely arrive for surgeries and procedures, and help pregnant women and those with newborns. The team also successfully secured stories in Spanish-speaking media outlets like Hoy En Espanol on ABC8.
VCU Health’s communications teams worked with ChamberRVA, the Virginia Hispanic Chamber of Commerce and others to ensure that information was available to employers and employees in both English and Spanish. And to spread the word to the area’s Latinx families, the team created a Spanish COVID-19 coloring book with the Children’s Hospital of Richmond at VCU, distributing 10,000 copies through multiple health departments and health care organizations across the state. Community partners are also printing and sharing the digital version of the coloring book.

As the world kept changing, we kept building.
The need for medical care became paramount — and our capabilities continued to grow, as we expanded in the communities we serve and set the stage for important new additions.

It’s the first of its kind in Virginia’s New Kent County: the new 17,000-square-foot VCU Health Emergency Center at New Kent is now open, offering around-the-clock, board-certified emergency medicine physicians, emergency-trained registered nurses, laboratory services and integrated technology.
The freestanding emergency center has the same capabilities as a regular emergency department and is the right place to treat true emergencies requiring immediate attention, such as a stroke, heart attack, serious burns, automobile accidents or bad falls. This full-service ER features 10 rooms, with two reserved for trauma resuscitation. It is not an urgent care center.
For patients treated at the center, transfers to VCU Health in Richmond and follow-up care with VCU Health services are all expedited. A separate entrance also leads patients to outpatient lab and diagnostic services.
The emergency center is located near Exit 205 off Interstate 64 at 2495 Pocahontas Trail, Quinton, Virginia.

In June of 2020, Sheltering Arms Hospital and VCU Health celebrated the opening of their new, collaborative destination rehab facility, Sheltering Arms Institute. The 114-bed, state-of-the-science physical rehabilitation facility is situated on 46 acres in the West Creek Medical Park, just west of Short Pump near the Broad Street Road and Route 288 interchange.
The new hospital combines the strengths of both organizations to provide exceptional care for individuals who have survived strokes, spinal cord injuries and brain injuries, as well as those in need of general rehabilitation for various illnesses and injuries.
“The opening of this new facility has been years in the making and we’re thrilled to now open the doors and provide a new avenue of access to leading-edge thinking, research, teaching and clinical practice,” said Paul Wesolowski, chief operating officer of VCU Health System.
The 212,063 square-foot-facility was constructed specifically for physical rehabilitation, with features including all private patient rooms, multiple specialty units, a 9,251-square-foot main therapy gym and three satellite gyms, research space, state-of-the-art patient care technology and rehabilitation equipment.
“Our vision is to reinvent rehabilitation for life beyond limits,” said Alan Lombardo, CEO of Sheltering Arms Institute. “This is an opportunity for all of us to serve the mid-Atlantic region and beyond.”

In early summer of 2020, VCU Health System celebrated the virtual topping out of the new 17-story, 615,000-square-foot Adult Outpatient Pavilion. Located on the MCV Campus, the pavilion will house a wide array of outpatient clinics and will feature a 472,000-square-foot parking deck with more than 1,000 additional parking spaces.
Most outpatient services provided downtown by VCU’s Massey Cancer Center will be consolidated in the new building, including medical, surgical and radiation oncology clinics and oncology infusion. The new pavilion will also house medicine infusion, women’s health services and a majority of the specialty outpatient clinics currently located at VCU Health’s Ambulatory Care Center, Nelson Clinic and North Hospital. Also included are an on-site laboratory, pharmacy and medical imaging service.
In addition to providing a space for leading clinical care, the building will feature innovative technology and collaborative spaces to enhance the research and teaching missions of both VCU and VCU Health.
The $383.9 million development is scheduled to open in December 2021.
Throughout the year, crews followed social distancing and protective equipment protocols to keep building a new home for children’s inpatient, emergency and trauma care, as construction of Children’s Hospital of Richmond at VCU’s new tower carried on.
The tower is being built adjacent to the outpatient Children’s Pavilion on the VCU Medical Center campus and will complete an entire city block dedicated to the care of kids. The new 500,000-square-foot facility will allow the pediatric team to provide world-class care for more children in our community — and in a welcoming environment designed just for kids and families.
Over the past year, the CHoR team has also continued to recruit top talent, develop programs to care in new ways and collaborate with community colleagues, and they have received exciting, national rankings for their urology, pulmonology, nephrology and cancer programs.
This is all possible with generous support from the community. To date, despite the challenging times of COVID-19, Children’s Hospital Foundation is $36 million on its way to an ambitious $100 million capital campaign goal to help fund the $400 million project.
Construction is on target with topping out coming in May 2021 and completion scheduled for spring 2023. There will be increased operating and imaging capacity, along with 72 private rooms in the new facility — 48 acute care and 24 intensive care. This is a 43 percent increase from CHoR’s current acute and intensive care bed capacity, with space to expand to 120 private rooms as needed to care for children from throughout Central Virginia, the commonwealth and beyond.
In a new era in health care, new leadership will guide us.
 As we continue to face new challenges, we also welcome a new CEO. Arthur L. Kellermann, M.D., M.P.H., became senior vice president for VCU Health Sciences and CEO of VCU Health System on Oct. 1, 2020. He is the first person in the senior VP and CEO role at VCU to have been elected to the National Academy of Medicine, with a distinguished career as a physician, epidemiologist, professor, dean, researcher and health policy pioneer. With Dr. Kellermann at the helm and 11,000 staff members charging forward, VCU Health proves that the future is all about resilience.
As we continue to face new challenges, we also welcome a new CEO. Arthur L. Kellermann, M.D., M.P.H., became senior vice president for VCU Health Sciences and CEO of VCU Health System on Oct. 1, 2020. He is the first person in the senior VP and CEO role at VCU to have been elected to the National Academy of Medicine, with a distinguished career as a physician, epidemiologist, professor, dean, researcher and health policy pioneer. With Dr. Kellermann at the helm and 11,000 staff members charging forward, VCU Health proves that the future is all about resilience.
The more we experience, the stronger we become.